A Silent Epidemic: Healing the Wounds of Native American Youth Mental Health
By [Your Name/Journalist’s Name]
In the vast, often unseen landscapes of Native American reservations and urban Indian communities, a silent epidemic casts a long shadow over the youngest generation. While headlines often focus on broader societal challenges, the mental health crisis among Native American youth remains acutely severe, marked by disproportionately high rates of suicide, substance abuse, and trauma-related disorders. It’s a crisis rooted in centuries of historical oppression, systemic neglect, and cultural erosion, yet simultaneously, it is met with profound resilience and a growing movement towards culturally informed healing.
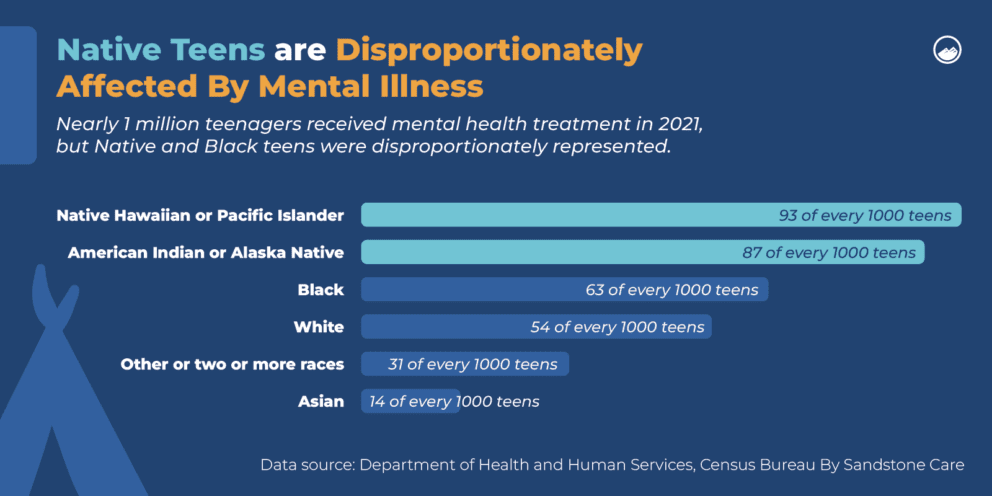
The statistics are stark and unforgiving. According to the Centers for Disease Control and Prevention (CDC), suicide is the second leading cause of death for Native Americans and Alaska Natives aged 10-24, with rates 2 to 3 times higher than the national average for their age group. Substance abuse, particularly alcohol and opioid addiction, plagues many communities, often beginning in adolescence and exacerbating underlying mental health conditions. Post-traumatic stress disorder (PTSD), depression, and anxiety are pervasive, reflecting a lived reality shaped by intergenerational trauma, poverty, discrimination, and a profound struggle for identity.
"We are dealing with the cumulative effect of hundreds of years of trauma," explains Dr. Lena Iron Cloud, a Lakota psychologist working with youth on the Pine Ridge Reservation. "The forced removal from lands, the boarding school era where children were stripped of their language and culture, the broken treaties – these aren’t just historical footnotes. They are living wounds passed down through generations, manifesting as complex trauma, distrust in institutions, and a deep sense of loss. Our youth carry this weight."
The legacy of the boarding school system, active from the late 19th century through the mid-20th century, is particularly insidious. Designed to "kill the Indian to save the man," these institutions subjected Native children to physical, emotional, and sexual abuse, forbidden from speaking their languages or practicing their spiritual traditions. The profound rupture in family bonds and cultural transmission created a void that subsequent generations inherited, leaving many youth disconnected from their heritage and without traditional coping mechanisms.
Barriers to Healing: A System Under Strain
Addressing this crisis is complicated by a labyrinth of systemic barriers. The primary healthcare provider for many Native Americans, the Indian Health Service (IHS), is notoriously underfunded and understaffed. Operating under a treaty obligation, IHS is meant to provide comprehensive healthcare, but its budget consistently falls far short of need.
"Imagine trying to serve a population with complex, intergenerational trauma and high rates of co-occurring disorders, in vast, rural areas, with the budget of a small city hospital," says Maria Tallchief, a policy advocate for tribal health initiatives. "Many IHS facilities lack the specialists, the beds, and even the basic resources needed for effective mental healthcare. Wait times for appointments can be months, and emergency services are often non-existent."
Geographic isolation further exacerbates the problem. Many reservations are remote, with limited access to roads, public transportation, or broadband internet, making it difficult for youth to reach mental health professionals, even if they were available. A critical shortage of culturally competent providers – particularly Native American therapists, psychologists, and psychiatrists – means that many youth encounter clinicians unfamiliar with their cultural context, history, or belief systems. This can lead to misdiagnosis, ineffective treatment, and a deepening of distrust in Western medical approaches.
"You can’t just give a young person a CBT workbook and expect it to work if they’re grappling with the spiritual ramifications of historical trauma or struggling to find their place in a world that often dismisses their existence," states Joseph Standing Bear, an elder and traditional healer from an Oklahoma tribe. "Healing for us is holistic. It’s about mind, body, spirit, and community. It’s about connection to the land and our ancestors."

Seeds of Hope: Culturally Informed Approaches
Despite the immense challenges, Native communities are not passive victims. They are at the forefront of developing innovative, culturally informed approaches to mental health that honor traditional healing practices and leverage community strengths. These initiatives recognize that true healing must be rooted in cultural revitalization and self-determination.
One promising model involves integrating traditional healers and practices into contemporary mental health services. This might include talking circles, storytelling, sweat lodge ceremonies, vision quests, or the use of traditional medicines. These practices offer a sense of belonging, connection to ancestral wisdom, and a spiritual framework for understanding suffering and resilience that Western therapies often lack.
"When I was going through a really dark time after my cousin’s suicide, I felt like no one understood," shares Aiyana, a 17-year-old Oglala Lakota girl now participating in a tribal youth program. "My school counselor was nice, but she didn’t get it. Then my auntie took me to a talking circle with elders. Hearing their stories, sharing my own, learning our songs – it felt like coming home. It helped me feel strong, like my ancestors were with me."
Telehealth has also emerged as a vital tool, especially in remote communities. While internet access remains a hurdle in some areas, expanding broadband infrastructure is critical for connecting youth to therapists and support groups who might be hundreds of miles away. This technology can reduce travel burdens and increase access to specialists, though it must be implemented with cultural sensitivity and awareness of digital divides.
Youth-led initiatives are another powerful force for change. Programs that empower Native youth to become peer mentors, mental health advocates, or leaders in cultural revitalization efforts foster agency and reduce the stigma often associated with mental illness. These programs build leadership skills, strengthen cultural identity, and create safe spaces for young people to discuss their struggles and find collective solutions. For instance, the We R Native campaign, an online health resource for Native youth, provides culturally relevant information and a platform for peer support, demonstrating the power of youth-driven content.
Tribal self-determination in healthcare is perhaps the most crucial long-term solution. When tribes have the autonomy and resources to design and manage their own mental health programs, they can tailor services to meet the specific needs and cultural values of their communities. This means moving beyond the limitations of IHS and towards a model where tribal nations are sovereign over their health and well-being. The Self-Governance program, which allows tribes to assume control of IHS programs, is a step in this direction, though it requires sustained and adequate funding.
A Path Forward: Investment, Respect, and Resilience
The journey towards comprehensive mental health services for Native American youth is long and complex, but it is not without hope. It demands a multifaceted approach built on several pillars:
- Increased and Sustained Funding: A significant and consistent increase in federal funding for IHS and tribal health programs is non-negotiable. This funding must be commensurate with the needs and treaty obligations, allowing for competitive salaries to attract and retain qualified professionals, expand facilities, and develop innovative programs.
- Cultural Competence and Workforce Development: Investing in training for all mental health professionals to understand historical trauma, cultural humility, and traditional healing practices is essential. Simultaneously, supporting Native American students to pursue careers in mental health, offering scholarships and mentorship, will build a workforce that truly reflects the communities it serves.
- Support for Traditional Healing: Recognizing and integrating traditional healers and healing practices into mainstream services, respecting their autonomy and wisdom, is vital for holistic care.
- Policy Reform and Tribal Sovereignty: Advocating for policies that empower tribal nations to exercise greater self-determination over their health systems, including direct funding and programmatic control, is paramount. This includes addressing systemic inequities in housing, education, and economic development, which are foundational to mental well-being.
- Community-Led Solutions: Prioritizing and funding programs designed and implemented by Native communities themselves, ensuring they are culturally relevant, community-driven, and youth-centered.
The mental health crisis among Native American youth is a profound challenge, but it is also an opportunity for justice and healing. By acknowledging the historical wounds, dismantling systemic barriers, and investing in the inherent strength and wisdom of Native cultures, we can help a generation not just survive, but truly thrive. As Dr. Iron Cloud puts it, "Our youth are not broken. They are resilient. They carry the strength of their ancestors. Our job is to provide the tools, the space, and the cultural connection for them to reclaim their healing journey and build a future rooted in their identity and power." The future of these vibrant cultures depends on it.


